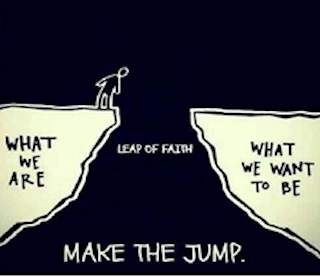
Go Ahead – Make the Jump!
by Caryn Unterscheutz*
 Every semester I ask my new students “What do you want to do with your lives?”
Every semester I ask my new students “What do you want to do with your lives?”
90 percent of them shoot their hands into the air with the exact same answer, “nursing.” We have a very competitive program at my university. Students who are not directly admitted to the program vie for a few openings in the nursing program in their sophomore year. Until then, they are enrolled in Community Health, Care Coordination, and Integrative Health degree tracts.
These Bachelor’s degrees are relatively new and are examples of the roles needed for the new healthcare workforce. We must change from the unsustainable healthcare delivery system we have now, to collaborative interprofessional practice where care is delivered in home and community settings. In a new randomized control study, 9 patients were assigned to home care and 11 remained in the hospital for treatment. Patients in both groups reported similar pain scores and patient satisfaction scores. Home patients experienced twice as much physical activity and a little more sleep than their hospital counterparts. The average cost of care for the home patients was 52 percent less than that of hospital patients. (Frellick, 2018) That is sustainable care.
Hospital nursing is and continues to be more technology oriented with machines providing the information we used to assess by touching the patient. Nurses look at a medical record computer screen, typing, while talking to the patient with no eye contact. We have less staff and higher acuity patients, time with each patient is limited, and we run around on 12-hour shifts with no time to eat, drink or use the restroom. Time and the art of caring appear to be lacking in the current model of hospital nursing. We hear what the patient is telling us, but do we really see the patient in all their humanity?
I recently sat for the Patient Advocacy Certification Board exam. My goal is to become board certified and develop an advocacy prep course for my students graduating with these new degrees. I believe the Patient Advocate role is necessary in our changing healthcare environment and provides an entrepreneurial opportunity if someone wants to be self-employed.
For example, Grandma and Grandpa live in Arizona. Their daughter lives on the east coast, with her husband and two kids. Both the daughter and son-in-law work full-time and the kids are involved in many after-school activities. Grandpa falls one evening and breaks his hip. Grandma rides with him in the ambulance to the hospital. Grandma has been showing signs of early dementia and relies on Grandpa to drive, shop, cook and clean their home. Their daughter calls a Board Certified Patient Advocate found on the AdvoConnection site who immediately drives to the hospital to meet Grandma and Grandpa in the emergency department. The advocate places a Skype call to the daughter, so she can see her father and mother and gain some peace of mind.
The days of the large nuclear family, living in the same region, are gone for many of us. It takes two incomes to support a family so when an emergency happens on the other coast, we are not able to drop everything and travel. The patient advocate fulfills a fundamental role in this scenario.
Grandpa is finally taken to his room and settled. He will have surgery the next day to fix his hip. The advocate makes sure the daughter is kept informed of the details. She has already arranged for a trusted home health aide to meet them at Grandma’s home. The aide will stay with Grandma overnight and make sure she is bathed and has had breakfast in the morning. The advocate confirms Grandma is comfortable with the situation before going home. Tomorrow, she will pick up Grandma and return to the hospital. The daughter is due to arrive by 5 p.m. and will immediately drive to the hospital. Grandpa has successful surgery to fix his hip and the advocate stays with them until the daughter arrives. Grandpa is scheduled to be transferred home the next day. The daughter and advocate meet to discuss next steps and to facilitate Grandpa’s recovery.
The daughter can only stay for one week, and when she leaves the advocate once again steps in to make sure all arrangements are in place and working. The home health aide will stay with Grandma and Grandpa. The advocate will make sure Grandpa continues his home physical therapy and accompany Grandma and Grandpa to follow-up doctor appointments. The advocate informs the daughter of Grandpa’s progress and will terminate the contract at an agreed upon time.
Lengthy hospital stays will become obsolete as we move healthcare forward to a community-based environment. Health care professionals in many rolls will be needed to sustain this paradigm shift. I see patient advocacy certification as a foundational cornerstone for many of the new healthcare roles as sustainable healthcare for everyone evolves. Patient advocacy roles will expand as clients realize their need to help navigate 21st century healthcare. Sustainable is not synonymous with simplified. The beginning of any change initiative is often riddled with complexity that dissipates as people become more comfortable with the change.
I realized after I took the exam that I have been advocating for patients for years. Now I advocate for students. Advocacy comes in many distinctive styles and colors but shares a common thread of caring. Active listening, eye contact, communication, touch, observation and visual cues are skills we used in nursing that are now often replaced by technology.
The patient advocate role is bringing care back to the chaotic healthcare continuum. The need for Board Certified Patient Advocates will quickly multiply, as public awareness grows about this profession.
Go ahead! Make the jump!
Reference:
Frellick, M. (2018) “Home hospital” halves costs in small randomized trial. Medscape 02/09/18.
Retrieved from https://www.medscape.com/viewarticle/892545
*Caryn Unterschuetz teaches at Arizona State University and is Coordinator of Internships in the non-clinical Baccalaureate Health Programs. She holds a master’s degree in Health Innovation and has been an RN for more than 30 years. She believes change is the only constant in life and works to influence change within healthcare and education.
— March 26, 2018
