As advocates, we all quickly become familiar with, and embrace, and share with clients, our Code of Ethics.*
Of course, there are many tenets to the code, but primary among them is the very specific statement and belief that while acting as a professional patient advocate, we will never make decisions for our clients. We work to help them make their own decisions, we respect the decisions they make, and we assist them to be sure they are carried out.
I’m sure, as you read that statement, you are nodding your head in agreement. YOU would never violate that tenet, would you? You are 100% committed to making sure your clients are making all their own decisions, even in difficult times.
And yet…
I received an email recently from a person who wants to start building an independent advocacy practice. In outlining her reasons for wanting to do so, she made this statement:
I am passionate about patient care and ensuring that quality vs quantity of life is always respected.
Pardon me, advocate, but your bias is showing! That said… I’m quite sure she would not recognize it immediately as being a bias.
Do you?
Well – it’s right there in black and white, “quality vs quantity of life is always respected.”
… I have to ask, what if your client wants a longer life at any expense? What if his preference is quantity, rather than quality? Do you then lack respect for that client? or do you try to change the client’s mind? or do you decide not to take that person as a client because you feel differently? (Do you even know what that person really believes?)
Pardon me, new advocate, but please take another look at our Code of Ethics! It’s not up to you to impose your preferences on your client. It’s incumbent upon you to ask questions, listen carefully, hear between the lines, and determine your client’s wishes. And then, of course, it’s up to you to help the client work toward his/her own preferences.
(I am sure that if I would point this out to our new advocate, she would immediately see where her bias was showing. And I’m sure she would agree that it’s not up to her to impose her own preferences. But it’s easy to see from this illustration how those biases creep into our work. So instead I’ll thank her for this excellent example!)
Imposing our own beliefs is often a result of a bias which cognitive psychologists call the “False Consensus Effect.” That is an internalized assumption that the world believes exactly the way we believe, which then gets imposed on others without recognition that is what we are doing.
 As professional, independent advocates, we need to constantly do a gut check on where our own opinions and preferences might be standing in the way of our professionalism. Any disconnect, “false consensus” or not, can result from making assumptions we should not be making. And you know what they say about assumptions!
As professional, independent advocates, we need to constantly do a gut check on where our own opinions and preferences might be standing in the way of our professionalism. Any disconnect, “false consensus” or not, can result from making assumptions we should not be making. And you know what they say about assumptions!
Other examples:
- Assuming that a patient should use insurance to pay for a drug; not realizing that oftentimes (mostly generic) drugs can be purchased for less in cash than using an insurance co-pay. (This needs to be called out to clients, then researched for each drug prescription.)
- Assuming that a client with great health insurance is getting great care, when the fact is that someone with great health insurance might instead get too much care – too many prescriptions, too many tests and procedures – all because whoever orders them can make money.
- Assuming a client has told us the truth about a situation he or she wants fixed, then moving forward as if the situation is exactly as described. we have learned over and over again that patients aren’t always truthful.
And this doesn’t even begin to touch the biases that might result from gender, race, or other attributes that we may or may not even recognize we have.
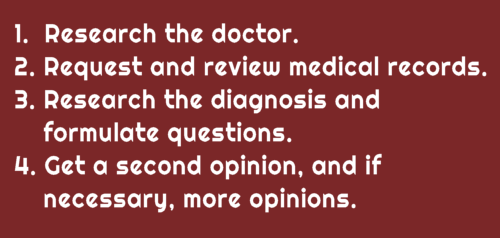
There are no simple solutions to this question of hidden bias except to suggest that we continue to question ourselves and our clients and listen carefully to the answers. For the new advocate I cited above, she will learn over time to ask her clients what their wishes are. Helping them organize their advance directives or make those end-of-life decisions may be quite eye-opening to her.

For the rest of us, it’s about staying open-minded, recognizing biases when we can, then questioning clients about their beliefs so we can serve them to our best ability within our advocacy Code of Ethics.
*There are three codes, all of which are identical in expectations, but which vary in their approach:
- Health Advocate’s Code of Conduct and Professional Standards? (developed by APHA, which you can sign at any time)
- The PACB Code of Ethics (which is tested during certification)
- The NAHAC Code of Ethics (which is required for NAHAC membership)
LEARN ABOUT APHA MEMBERSHIP | MASTER LIST OF PRACTICE RESOURCES | ONLINE COURSES TO LEARN ADVOCACY



Thank you for the reminder to always look to our motives when helping our clients.