You have probably heard that old joke about a Boy Scout who was determined to help a little old lady cross the street. After a number of attempts and iterations, he finally picked her up and carried her to the other side of the street, set her down on the sidewalk, and left, having completed his good deed.
But the joke was really on him – because the lady had no interest in getting to the other side. She had wanted to stay right where she was.
We frequently receive requests to take Granny across the street. They come in the form of Unmet Needs requests from well-meaning friends and family who want an advocate to help someone they care about.
Too many of those patients are just like the little old lady, and too many advocates are trying to play the role of the Boy Scout.
How?
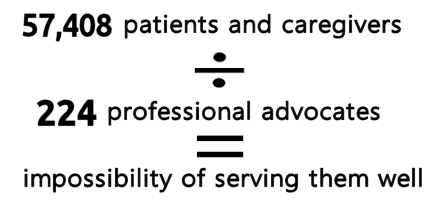
What we know is that not all patients want an advocate. This has nothing to do with need; I think we can agree that almost every patient NEEDs an advocate. But for many reasons, if a patient doesn’t want help then it should not and can not be forced on him or her – no matter how family or friends feel about it.
Yet, every day we get calls, or email outreach, or inquiries in some fashion from well-meaning friends and family. Here are examples from a glance at the Unmet Needs List:
- My friend has chronic lyme disease. She is at the end of her rope. She needs a person to help her In so many ways…
- My mother has been in the hospital for the past 5 months. She has been seen by multiple doctors, and all are unsure what is causing her confusion…
- Looking for advocate to assist 60 year old man with mood disorder navigate through paperwork, treatments, etc…
- My son is in the hospital in critical condition. He’s being mistreated…
- My friend and coworker’s brother ( only living immediate family) has been diagnosed with lung cancer and has become, just in a matter of weeks has become mentally unstable…
- … and many more.
You have probably heard similar stories during phone calls or in email. Someone calling you in hopes you will help someone else.
Here’s the problem: Many of those patients, like the little old lady, don’t want help; they don’t want an advocate. Further, and important to us as private, independent advocates, not all these patients are willing to PAY an advocate.
Now – agreed – they probably need an advocate. They certainly deserve one. An advocate can improve their journeys and outcomes. But for their own reasons, they don’t want one or don’t want to pay one. That’s just the way it is.
So how do we respond to these kinds of requests from a patient’s friends and loved ones?
 It’s not difficult. But there are definitely some determinations to make at the outset of a conversation.
It’s not difficult. But there are definitely some determinations to make at the outset of a conversation.
Here’s an example of how that conversation should go:
~ Family member: “My mom needs an advocate. She lives too far away for me to help her and she can’t do this alone.”
~ You, the Advocate: “Has your mom indicated to you that she would like someone, an advocate like me, to work with her?”
~ Family member: “No. But she’ll be happy to know you can help.”
~ You, the Advocate: “Is she able to discuss this with me by phone herself?”
What you’re hoping to determine here is whether the mother knows that the adult child is looking for assistance, and how receptive the mother is to the idea of outside help. If Mom doesn’t know what’s going on, that may be a red flag to you, the advocate. You’ll need to discuss how to make the connection. The BEST way to do that is to ask that the mother call you directly, or to be on a three-way call with the adult child and you.
~ You, the Advocate: “I’m sure you understand that since I’m an independent advocate, I charge for my services (just like a lawyer charges for services). Is she willing and able to afford my services?”
~ Family Member: “I’m not sure. I don’t know if she can afford your services, and I sure can’t. How much do you charge?”
This is the second important determination. So often the loved one or friend thinks an advocate is a great idea – but has no idea how your services will be paid. The possible answers here are “yes”, or “no”, or “I will be paying for your services.” Their response will provide you with answers you can use to decide your next steps. Any indication that no one has the resources and is willing to pay will be a red flag, of course. Further, the question about how much you charge will naturally follow, and you’ll need to invoke whatever your canned speech about cost is. (And don’t forget my always-admonition: never provide an hourly rate in isolation!)
My final piece of advice on this topic is this: YOU should never be the one to initiate a phone call or email to a patient who hasn’t contacted you directly first. If a friend or family member asks you to place the call or to send the email to the patient – don’t do it. You might be blindsiding a patient who can’t or won’t discuss private health matters with you and that’s a sure way to create a problem for everyone, including yourself. Let whoever did the initial outreach (whether they did so through the Unmet Needs list, or by direct contact with you) set up the introduction to you, preferably by phone for at least the first time.
Don’t forget: It’s always possible that the Granny-patient doesn’t really want to cross the street!
Have you had experience with any aspect of these someone-other-than-the-patient requests? Share your story with us – and please share your own DOs and DON’Ts to help others.
MASTER LIST OF PRACTICE RESOURCES | LEARN ABOUT APHA MEMBERSHIP | REASONS PATIENTS NEED ADVOCATES





This is so true Trisha! I have had so many calls that are for a family member or friend. I usually start off by allowing them to share what is going on. This will help me to see if it is an area that I can assist with. If I feel that it is an area where I can be helpful, I then ask about the knowledge of the primary client who is the primary beneficiary of the services. I say something like, “Is Mr. Jones aware that you are looking for an advocate?” If they say, yes, then I try to get a sense of how do they feel about it? 9 time out 10, the response is “Well, yes but they are somewhat resistant.” I tell them how I can help but I would need to speak to the primary client first because they would have to sign paperwork first before we can get started.
Now if somewhere it is believed that the person isn’t able to speak on the their behalf due to disability or medical condition, then I ask who is the POA. That is when I will take information and signatures from the secondary client. I have had several situations where the payee is the secondary and primary isn’t. That is fine and more than normal usually the case.
I have been able to give a client a “taste” of what I can do – not for free- so that can see how an advocate can make a difference. It has worked once. It usually is that they either do or they don’t. The ones that do are educated and aware of healthcare advocacy. That is why we need more education for patients and the public.
My experience with these scenarios are much as Trish describes: a desperate family member collecting information for a struggling loved one. My ” Do’s” for these are : validate the difficult emotional state of the person contacting you, educate about what advocates can do to help, give the canned speech on my costs( which I seem to tweak each time I have these calls). Then, adopt a ” come what may attitude”. If the loved one is both able to pay and in a healthcare mess, I am confident they will contact me. If not, then hopefully, I have advanced the general public’s understanding of an advocate’s role.
I also keep a ” potential client ” call log, then if there is follow up, I can readily reference the information received from that initial call.