My husband and I moved two years ago to Florida where we now live in an “active adult” community*. We love it! We’re very happy here. We’ve met and made many new friends – people we have truly come to care about.
I’m following in family footsteps. My parents did the same thing decades ago. They lived in a different city, but they, too, lived in an active adult community for 20+ years.
My father, in a somewhat macabre voice, always called it “God’s Waiting Room.”
And, as I learned again this past week, it turns out that we now live in God’s Waiting Room, too.
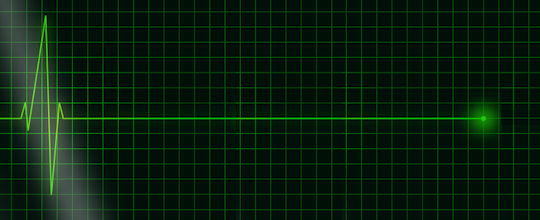
One evening last week a neighbor phoned, informing us that our friend who I’ll call Sam, a fellow we’ve gotten to know and enjoy, had suffered a heart attack, and had subsequent surgery after coding in the hospital waiting room. Sam was in a coma, and we wouldn’t know for several days whether he would pull out of it, and whether there was any long-term brain damage.
As of today, we still don’t know. Sam is still in a coma.
Now – in God’s Waiting Room this is not unexpected. In less than two years, this is our third such experience, having already lost two friends who have passed away. It’s not a question of if or when. It’s a question of WHO.
Of course, I could begin an entire riff on why a private advocate could succeed in this community, but that’s not today’s post.
No, today’s post is about taking someone’s life into your hands because you don’t know what to do in such an emergency.
I’m writing this post because I’m angry, frustrated – and so very sad. Here’s why:
The neighbor who phoned us (we’ll call him Tom) lives next door to Sam. It seems Sam, who lives alone, and experiencing frightening symptoms, appeared at Tom’s door that morning and asked Tom to take him to the hospital. So Tom drove Sam the 10 miles to our small community hospital, then sat with Sam in the waiting room for 15 minutes until all of a sudden Sam clutched his chest and fell forward out of his chair, coding right there in the ER.
Of course the ER personnel jumped in, saved him using the heart paddles, then swept Sam off to surgery…. leaving us to wait it out to see if Sam can recover.
WHAT’S WRONG WITH THIS PICTURE? So many things…
For starters, even though Tom meant well in transporting Sam to the hospital, he should instead have dialed 9-1-1 so the professionals would have done the transporting. Sam would have received care from the moment the EMTs arrived. No waiting! With that immediate care, it’s entirely possible they could have prevented Sam from coding at all and his survival would not have become this question mark.
 Second: Tom didn’t realize that the local community hospital is among the LAST places any of us in this area should go for cardiac emergencies. Even if Tom didn’t realize Sam was having a heart attack, he should have known (and knows now) that the larger hospital, just 8 additional miles away, is well-known for its heart and stroke care. A much better choice!
Second: Tom didn’t realize that the local community hospital is among the LAST places any of us in this area should go for cardiac emergencies. Even if Tom didn’t realize Sam was having a heart attack, he should have known (and knows now) that the larger hospital, just 8 additional miles away, is well-known for its heart and stroke care. A much better choice!
Patients can request EMTs take them to their choice of hospitals. Yes, it’s possible the request won’t be fulfilled if that hospital’s ER is full, but it’s certainly worth asking, and in the scenario where Sam was still conscious, that request could have been made.
The Bottom Line – dialing 9-1-1 would very likely have improved Sam’s chances.
Now Sam’s future is a huge question mark. Tom has to live with the fact that he made a bad choice which may ultimately mean Sam crosses that very, very thin line between life, quality of life, and death.
What Can Patient Advocates Learn from This?
There are a few things patient advocates can do for their clients, their practices, and their own loved ones that can be learned from this event.
It begins with making sure everyone you talk to is aware of the folly of driving someone, including themselves, to the hospital when faced with even a possibility of life-threatening symptoms.
Yes, I do realize that the new reality of payment systems may mean we have to pay out-of-pocket for a paramedic transport to a hospital. But when it may mean the difference between life and death, it’s a very small price to pay.
_______________
For Our Practices
Medical Emergency Preparedness is an excellent topic for blog posts, or public speaking opportunities. You can provide the same information I’ve provided above. You can develop and share printed or digital lists of emergency steps adding your own logo and contact information.
_______________
For Our Clients
Help clients prepare for an emergency, especially if you work with older clients who could have a heart attack, or a stroke, or any of dozens of “events” that would require a quick trip to the hospital. Do they need to dial, or can they text 9-1-1? If they use a cell phone, can they be located by dispatchers? or do they need a landline?
Help them put together the information the paramedics and hospital may need: doctor’s names and phone numbers, conditions they have, lists of drugs they take, first of kin and emergency contact information, copies of (or the location of) their advanced directives… Many communities have a system in place where the paramedics know to look on the refrigerator, or inside the refrigerator door for access to this information.
ICE: In Case of Emergency – for those clients who have cell phones, they can designate someone in their contact list as ICE – and if their phone is found nearby, EMTs, firefighters, or police know to look for the ICE contact. There are apps, or some phones come with ICE built in – just add the person’s specific ICE information.
There may be more you can do for your clients to help them prepare. Even if they never need this help, it will provide great peace-of-mind to know it’s in place.
_______________
Emergencies can, do, and will happen! Be sure everyone around you, whether or not they are clients, prepares for an emergency and knows what to do.
Don’t let friends OR family OR clients (or YOU!) decide against dialing 9-1-1.
DO NOT BE TOM!
*No. We do not live in The Villages! I wish I had a nickel for everyone who asks 🙂
LEARN ABOUT APHA MEMBERSHIP | REASONS PATIENTS NEED ADVOCATES | MASTER LIST OF PRACTICE RESOURCES



This is a great example of understanding the basics can go a long way!